emergency departments
The Front Door During a Crisis
The mantra in the emergency department is, “your once-in-a-lifetime is our every day.”

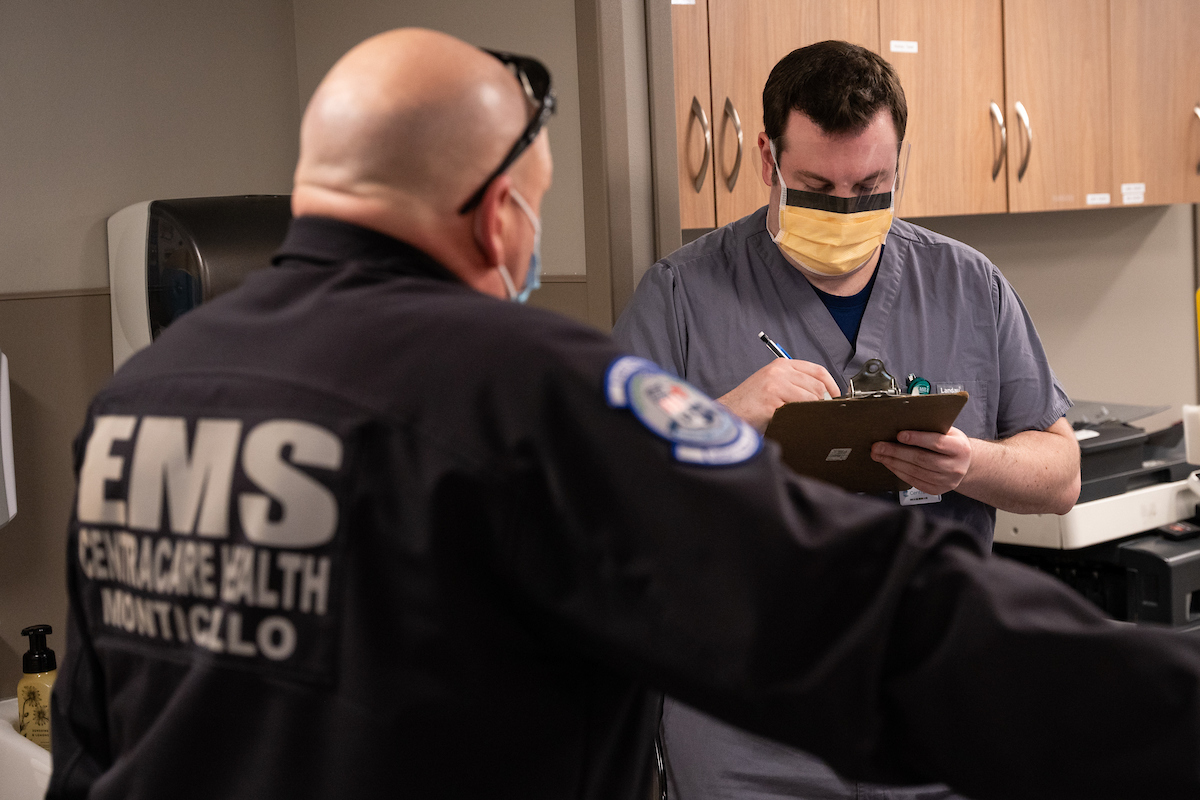
Emergency Department (ED) staff are, by nature of their work, used to dealing with acute medical situations of every kind. But they’re not typically with any one patient for very long. The surges of COVID patients changed that, as beds filled up in the rest of the hospital.
“We deal with the first 90 minutes of an illness,” explained ED Medical Director Kurt Belk. “We ‘stabilize and admit’ or ‘stabilize and transfer’ or ‘stabilize and discharge.’ But for parts of the pandemic we were inpatient providers, providing 24/7 care sometimes for several days.”

With support from hospitalists and intensivists, the ED staff adapted to provide ongoing care management for patients who had nowhere else to go. But that in turn created a backlog of patients awaiting emergency care.
“We are the only place in the hospital that can’t say ‘no,’” said Belk. “Upstairs can say ‘no, we’re too full,’ ‘No, we’re too busy.’ The ER cannot do that. And we never do that, ever.”


Real-time response


Working with 3M, St. Cloud Hospital developed a triage area where ED staff were able to separate out COVID and non-COVID patients.
“One of the bigger challenges of COVID is people still have heart attacks and strokes and GI bleeds,” explained Belk. “And some people just have COVID. And you certainly don’t want to have your other ER patients mixing with your COVID patients so that everybody gets infected.”
Amidst the stress, there were welcome surprises. Ken Flowe, MD, an ED physician in Willmar, says medical care practices are developed to treat the worst case scenario. But different patients exhibit different levels of resilience to the same injury or illness.

“We had people survive that shouldn’t have survived,” said Flowe. “There have been patients with heart attacks that I would normally have called a helicopter for and immediately sent them right to a cath lab. That couldn’t happen, but they didn’t suffer. And then we had people with severe head injuries that were thought to have an unsurvivable injury, who were able to leave healthy and walk out of the hospital. So sometimes worst-case scenarios happen, but they don’t always happen.”
And then there were those patients who looked fine, but were quite the opposite. ED nurses had to adapt to diagnosing patients whose symptoms were completely different from the norm.
“We had many patients that would come in and they were extremely hypoxic, but they were walking and talking,” recounted ED RN Jake Heins. “Pre COVID, that patient would have been unresponsive; their oxygen sets are so low that they wouldn’t be alert, and now they’re physically walking up to the desk.”



Added stress

ED Nurses also had to deal with increasingly volatile patients and families.
“When I started nursing 40 years ago, if you would have told me that patients would be talking to medical staff and acting and treating medical staff in the manner that they are, I would have said that you were completely insane, that we would never see that,” said ED RN Deb Schaefer. “I’m actually seeing that now on a constant basis. It’s daily – it’s not even weekly or monthly – it’s on a daily basis, from the verbally abusive patient out in triage to the actually physically aggressive family member, punching people.”
COVID took an already stressful job and raised the stakes even higher. Jason Foos, Interim Director of the ED at St. Cloud Hospital, says that took a toll on the staff.

“One thing that I would have done differently or better, if I could wave a magic wand, is support the team members better,” reflected Foos. “I think we did a pretty good job – answering questions, being present from a leadership standpoint, trying to allay fears, and providing the right resources. But I don’t think there’s ever an upper limit on appreciation and support that you can provide to people doing the work day to day.”
For ED Medical Director Kurt Belk, working through the pandemic has underscored the importance of having a strong team.
“The mantra in the emergency department that we have to remind ourselves is, ‘your once in a lifetime is our every day.’ We see everybody’s worst moments, and that does have an accumulative effect. And it’s leaning on each other that gets you through that – the fact that you have your ER family that you’ve developed these relationships with, these bonds with – that’s why you go to work and do what you do.”