March 23, 2021
Tom’s Blog: Changes


As most of you are aware, The Centers for Medicare & Medicaid Services (CMS) made significant wRVU changes for 2021 outpatient evaluation and management (E/M) codes with implications to documentation and reimbursement. Since the vast majority of physicians and APPs utilize these codes, it is important that all of us understand what this means – for both ourselves, and our group practice.
Dr. Jessie Roske and her team have been working to translate the documentation guidance from CMS into real world advice, and I hope that you have been able to attend one of her education sessions. As she has stated, the good news is that the intent of these changes by CMS has been to decrease the burden of documentation and to reward medical decision making rather than ‘checking boxes.’ My own view is that this should ideally minimize distance from our purpose and recognize our value by rewarding what we do – utilize our knowledge and experience to serve patients.
The stated intent of the adjustments was the recognition that a large amount of work in the outpatient setting was being inadequately addressed in the previous system.
In this writing I will focus on the wRVU and reimbursement changes that we introduced in the podcast interview with Tom Feldhege and Joe Blonski. The E/M changes have made journal headlines because unlike the small changes in typical years, CMS introduced major wRVU valuation alterations in tandem with the coding guidance just mentioned. The stated intent of these adjustments was the recognition that a large amount of work in the outpatient setting was being inadequately addressed in the previous system. Although these changes apply independent of specialty, they more heavily impact those disciplines that utilize certain outpatient E/M codes more frequently, particularly primary care.
As I have mentioned previously, because CMS is required by statute to maintain budget neutrality, this increase in wRVU values was paired with a decrease in the conversion factor (decreased by $3.68 to $32.41) that CMS utilizes to reimburse organizations for professional services provided. The result—when comparing the same work against the new wRVU values—was an overall increase of 8.1% in physician wRVU with a range of 0-28% by specialty for our organization (results will vary based on the mix and number of specialties and their use of outpatient codes). It is important to note that the 8.1% increase is to the total wRVU values, not the actual reimbursements received from CMS. In other words, while the amount of wRVUs would increase, the dollars of reimbursement would not.
Budget Neutrality Factor
Because of the budget neutrality factor (no new revenue), I think it is apparent that this holds the potential to be a divisive issue amongst partners. As I mentioned in a previous writing, I believe that physicians whose primary revenue is from procedures would support increased compensation for their partners who focus primarily on outpatient E/M services but would be unlikely be interested in experiencing a reduction in compensation to support that change.
The senior executive team decided to increase total compensation in the physician program by 2% — aligned with market estimates — which will total $2.3 million in FY22
Given all of this, we set to work on developing our approach for FY22, beginning on July 1, 2021. First, the senior executive team determined that we would increase total compensation in the physician program by 2% — aligned with market estimates — which will total $2.3 million of additional expense in FY 2022. We then asked the Physician Compensation Advisory Committee (PCAC) to work with us to determine how best to approach this challenge within the parameter. As a first step, the PCAC developed four guiding principles for our approach:
- Recognize the intent of CMS to increase the reward for E/M work
- Acknowledge that CMS is rebalancing reimbursement, not increasing total reimbursement
- Be feasible from a financial standpoint
- Be cognizant of national and regional market approaches
- Result in an acceptable pace of change
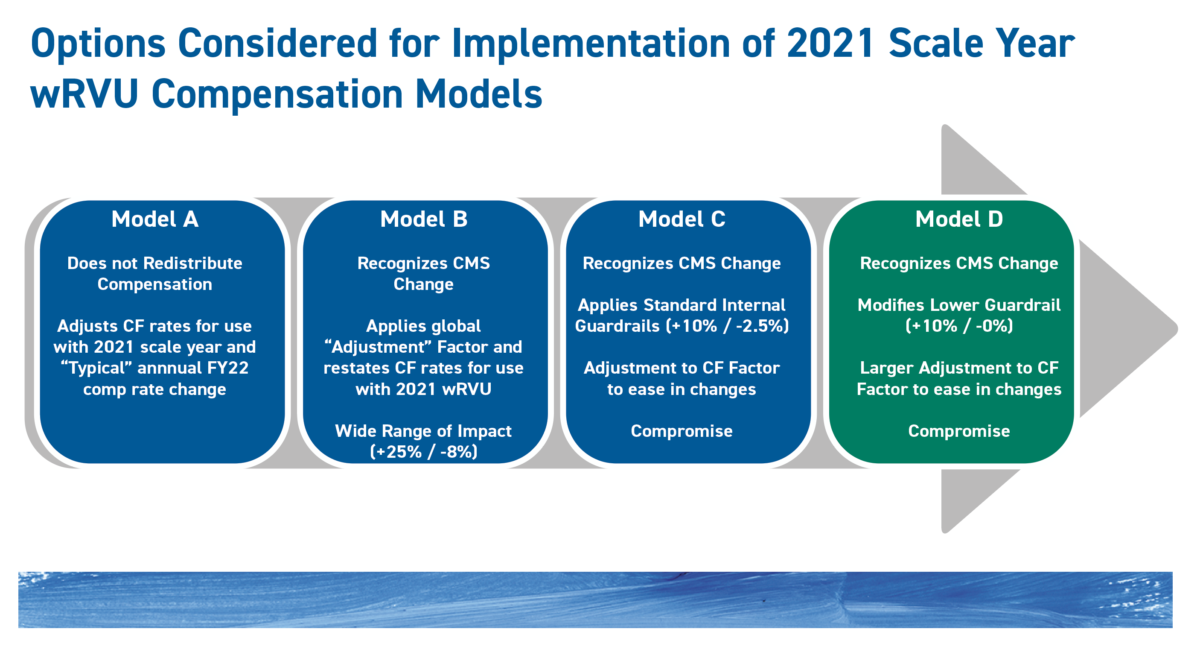
With this in mind, four models were developed by Tom Feldhege and his team:
Early in the discussions, PCAC dismissed maintaining the 2020 wRVU values and FY21 conversion factors (CF) for FY22, as that approach did not support the first guiding principle of recognizing CMS’s intent. It may be a surprise to some that this was a consideration at all given that it makes no adjustment for CMS changes and continues to utilize the 2020 wRVU values. Sullivan Cotter and Associates informed us that this has actually been the choice of a number of organizations around the nation for 2021.
- Model A implements the new 2021 wRVU values but does not reallocate compensation among specialties, as will occur with CMS reimbursement.
- Model B recognizes the CMS change and applies a global adjustment factor across specialties to keep the annual increase in compensation to $2.3 million, but with no upside or downside guardrails. (The incremental cost without the adjustment would be $11 million.) As you can see from the image above, this would result in a potential swing of +25% to -8%.
- Model C applies guardrails of +10% & -2.5%.
- With Model D, the guardrails are set at +10% and -0%. (A variation of Model D with guardrails at +5% & -0% was also considered.)
Decision
Ultimately, we in the PCAC chose Model D as we felt that this option best supported the guiding principles noted above. Namely, Model D provided up to 10% upside for those benefiting from the wRVU changes and 0% downside for those adversely impacted by the E/M changes. It should be kept in mind that this is a year-by-year process that will be influenced by the national and regional market trends, as well as future changes by CMS. It is anticipated that the private payers will follow the lead of CMS as they have in the past. Over time, this will likely result in an ongoing re-weighting of the wRVU schedule.
In the weeks ahead, PCAC will be working through a number of secondary decisions such as the approaches to wRVU thresholds and compensation amounts in tiered compensation and salary-plus models for certain departments.
Understandably, some people will disagree with the decision regarding which model was chosen. Although it was not explicitly stated in the guiding principles above, I am confident that everyone involved in this process had this thought upon their mind: what we decide needs to pull us together rather than apart as a group practice.
Please let me know what you think about that and let’s keep talking.
Tom

