April 16, 2021
Explaining the Guard Rails
Implications of Changes to Evaluation & Management Codes
Background
Each year, the Center for Medicaid Services (CMS) updates the physician fee schedule. Normally it includes very small iterative changes, but this year major changes were made to the Evaluation and Management (E&M) codes. E&M codes are primarily used in outpatient clinic visits, which are more heavily used in primary care. CMS has assigned significant increases in work RVU values for these codes, while at the same time — in an effort to achieve budget neutrality for the government — decreased the conversion factor for what they actually pay.

The Process
Because of the budget neutrality factor, compensation could actually decrease for people who don’t utilize these codes frequently. Our task as colleagues and a large group practice was to hold conversations and deliberate together in order to find an equitable solution.
First, CentraCare allocated a 2% annual increase in physician compensation, consistent with past practices. Then, the Physician Compensation Advisory Committee (PCAC) took up the task of determining how to implement the CMS changes to the E&M codes.
The committee began deliberations with a set of guiding principles:
- Recognize the intent of CMS to increase the reward for E/M work
- Acknowledge that CMS is rebalancing reimbursement, not increasing total reimbursement
- Be feasible from a financial standpoint
- Be cognizant of national and regional market approaches
- Result in an acceptable pace of change
Four models were constructed and evaluated as options for implementation:
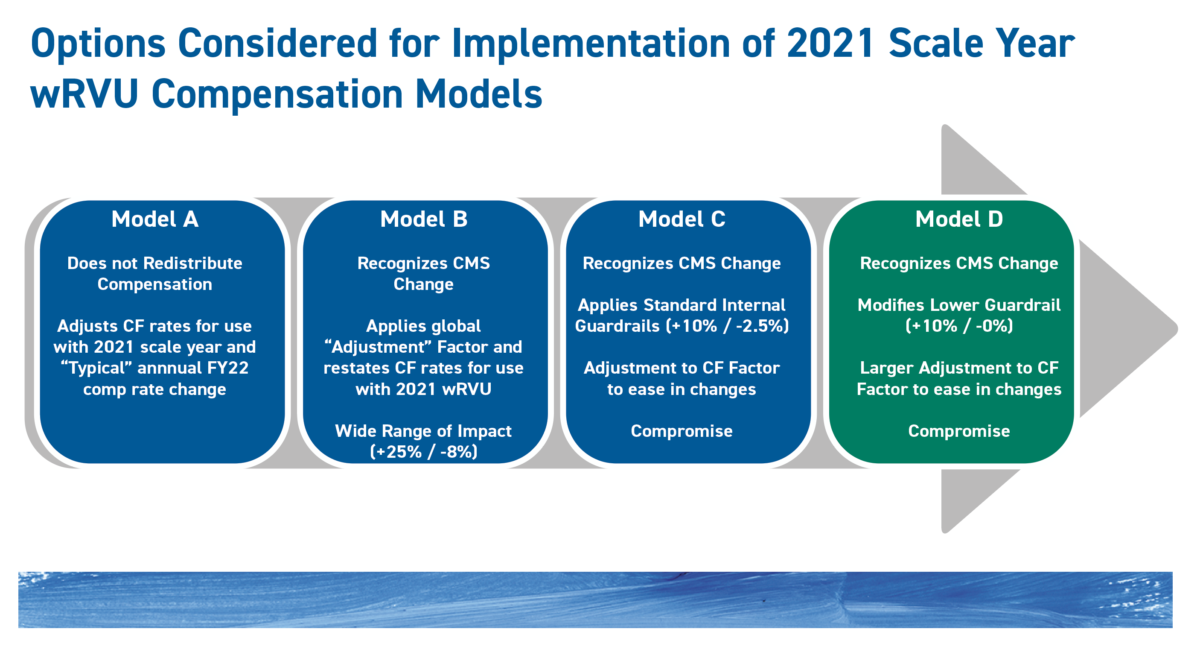
Model A:
Implement the new 2021 wRVU values but do not reallocate compensation among specialties, as will occur with CMS reimbursement.
Model B:
Recognize the CMS change and apply a global adjustment factor across specialties to keep the annual increase in compensation to $2.3 million, but with no upside or downside guardrails. (The incremental cost without the adjustment would be $11 million.) This model would result in a potential swing of +25% to -8%.
Model C:
Apply guardrails of +10% & -2.5%.
Model D:
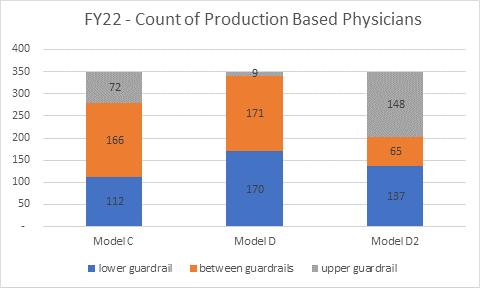
Apply guardrails of +10% and -0%. (A variation of Model D with guardrails at +5% & -0% was also considered.)
The Take-away
“When the PCAC started to look at this situation, our intention was to find an equitable way of applying the changes without impacting anybody too negatively,” explained Dr. Ben Haeg, a member of the PCAC committee and primary care physician at Sauk Centre. He continued, “The system compensation plan itself has built-in guardrails so that no individual group’s compensation goes up by more than 10% in a given year. And there’s a negative guardrail for not going down more than 2.5% in a year.”
When the committee evaluated the four models, Model A did not meet four of the five the guiding principles. While it recognized the intent of CMS to increase the reward for E/M work, it failed the other tests of the guiding principles. Model B satisfied the first three guiding principles, however, it failed to account for the guardrails in place that prevents an individual group’s compensation to increase by more than 10% or decrease by no more than -2.5%.
PCAC’s recommendation of Model D led to a decision to adopt top and bottom guardrails of +10% and -0%. The 2% system increase in physician compensation—roughly $2.3 million—will be shared more generously by primary care physicians because of the CMS changes. Compensation for procedural specialists, whose compensation could be negatively impacted by the CMS changes, will be protected in the new fiscal year with the bottom guardrail of -0%.
As we interpret market data in the next couple of years, adjustments may be required to continue to move toward the intent of the CMS changes.
Dr. Ben Haeg, Member of the PCAC
“Our compensation plan is based on market medians,” said Dr. Haeg, “and the information from the COVID year is going to be very difficult to interpret. The information from the first couple of years of the CMS changes will also be difficult to interpret. So, we’ve come up with a plan that PCAC is comfortable with and we’re confident is good. But what happens in the second and third years will matter a lot. As we interpret market data in the next couple of years, adjustments may be required to continue to move toward the intent of the CMS changes.”
By Comparison
The CMS final decision was released in December 2020. CentraCare’s fiscal year, like many non-profits, begins July 1st and ends June 30th. Changes to compensation plans occur at the start of a new fiscal year. By contrast, other healthcare systems may run on a calendar year fiscal year. Many in our peer group, according to our national consultants, are waiting to implement the CMS changes on January 1st, 2022, when their next compensation plan rollovers occur. CentraCare is implementing the compensation changes at least six months earlier than many other groups in Minnesota.
Additional Information
Clinical Partners Physician—APP Leadership Meeting, April 6th
CMS E&M Changes 2021 with Greg Von Elbe, Tom Feldhege & Tom Schrup
Implementation into FY22 Physician Compensation
Slides from Physician-APP Leadership Meeting, 4/6/21
Clinical Partner Podcast with Tom Feldhege, Dr. Joe Blonski & Dr. Tom Schrup:
Implications of the Evaluation & Management Code Changes