Intensive care

Adapting to change in the ICU
Change is constant in healthcare, but the pandemic has been like nothing else.
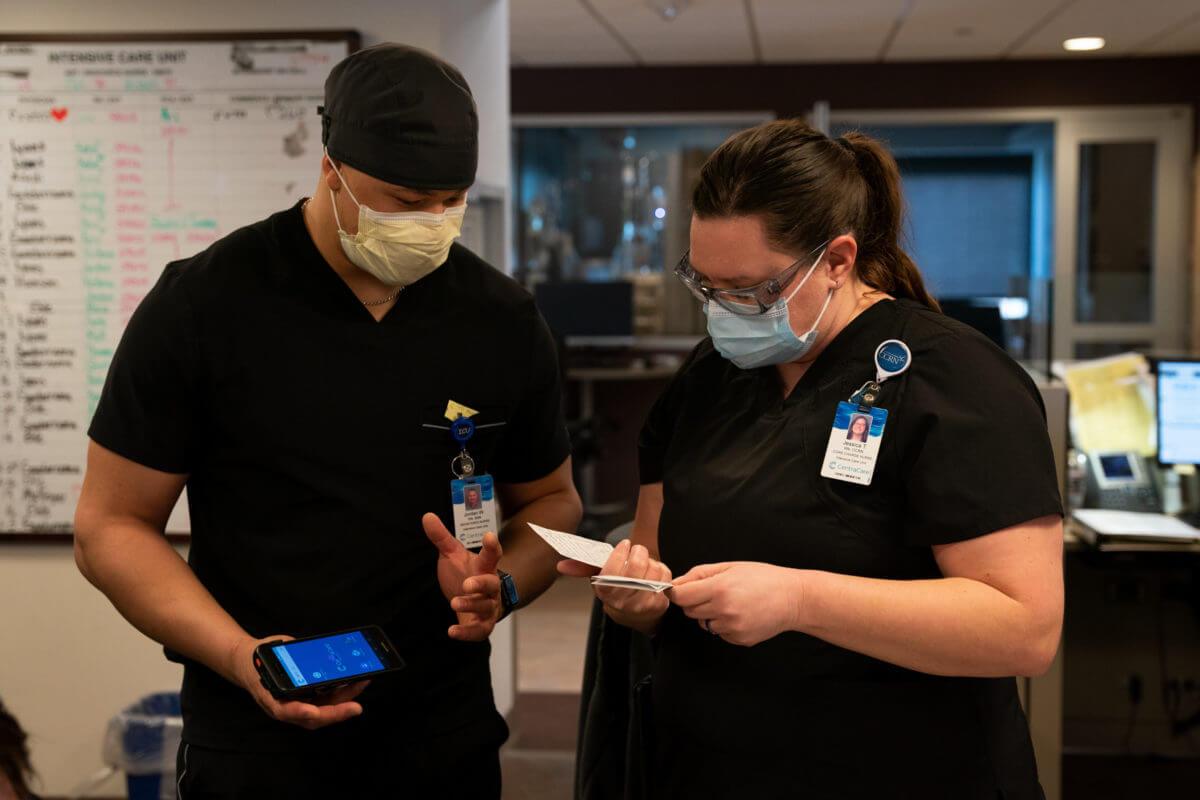
“In the last two years, things changed exponentially faster than anybody could have ever guessed,” said Jessica Tindal, RN and core charge nurse in the ICU at St. Cloud Hospital. “Somehow you just roll with the punches.”
And that’s what the ICU team did through all the ups and downs and seemingly endless surges.


Michelle Gamble, Director of the ICU, was just a few weeks into her new role when COVID was first detected in the U.S. “I had worked in the ICU since 2000 in different capacities, but I don’t know that I was ever going to be prepared for what was ahead of us.”

New viruS,
new staff


Intensivist Tim Ehle, MD, had just transitioned to critical care full time in the ICU when concerns about COVID surfaced. “I remember thinking to myself, ‘My God, what did I sign myself up for,’” said Ehle. “Early on, it was a lot of worry about the unknowns and it was a lot of learning on the fly.”

Dr. Jack Lyons joined CentraCare and the ICU team in September 2019. “My wife is a trauma surgeon so we were both just getting our feet wet and getting established in the community when COVID hit,” he said.



Team players

For Michelle Gamble, it was about being a team player.
“Like many departments across CentraCare, the ICU team is a family,” she said. “It’s a lot of work, it’s nonstop, and everyone has each other’s back. There are ups and downs, but through it all we’re a team.”
Early in the pandemic, being a team player meant assigning some of her staff to other areas of the hospital that needed help with critical care due to the pandemic. “It was difficult when we had to move staff to address the crisis we were facing,” she added. “But we did what we had to do to care for our patients.”

As the pandemic spread, so did the need for ICU resources.
“We were fortunate to have a lot of extra hands on deck, which were all lifesavers,” said Dr. Ehle. “We had more patients than we had intensivists, pulmonologists and hospitalists to take care for them. We were blessed to get help from anesthesia, nurse anesthesia, Advanced Practice Providers (APPs) and Palliative Care to name a few. And I can’t say enough good things about the nurses who cared for COVID patients.”

Thomas Miller, RN, joined the team in November 2020 after graduating in the spring of that year. “It’s been a grind, but I’m extremely blessed to be where I am,” he said. “I believe this experience has made us better nurses, but at the same time, it doesn’t make our lives easier. I’m just thankful for the staff around me, like our nursing assistants. They are fantastic and they too were thrown into tough situations, but we all had faith in each other.”


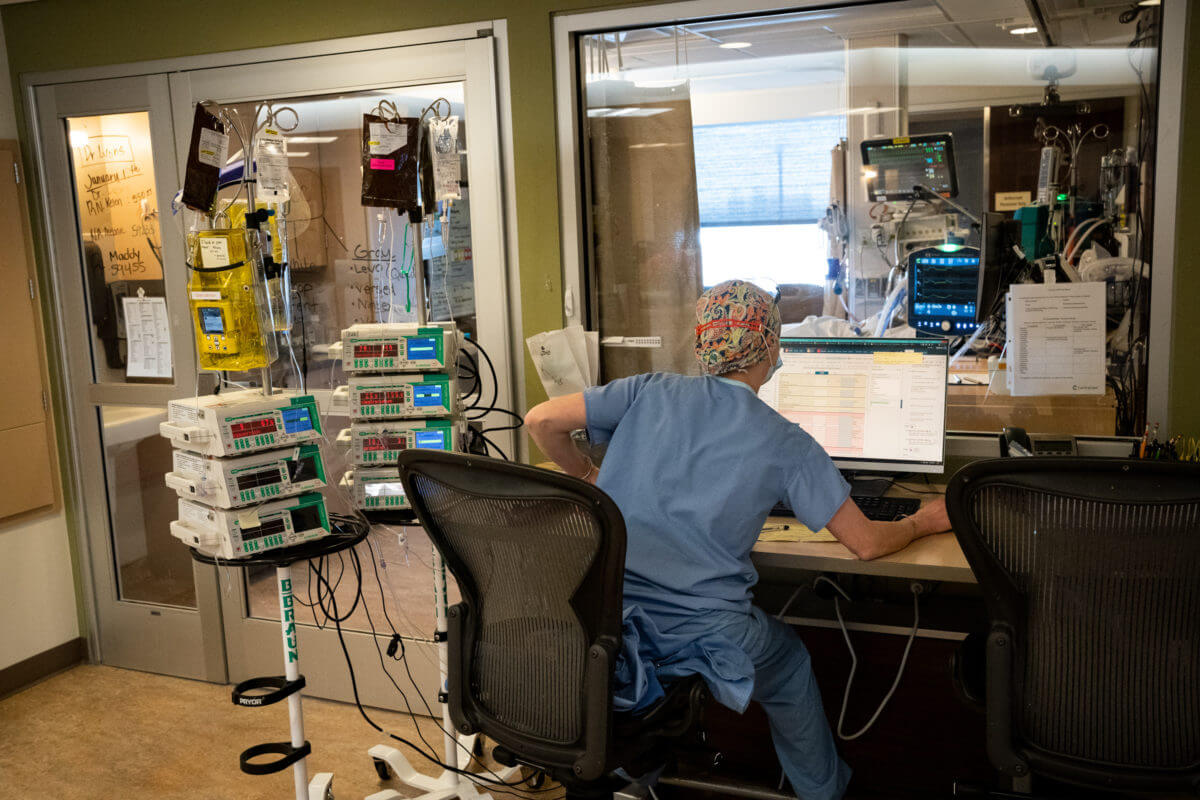
Plugged-up lungs


“The most common procedures we were doing were bronchoscopies, which basically puts a camera into somebody’s lungs,” said Dr. Ehle. “The toughest thing about managing COVID is any improvement takes a very, very long time. Often people would be on the ventilator for weeks and inevitably they would develop bacterial pneumonia which would plug up their lungs. So patients often needed frequent bronchoscopies to get cultures to suction out mucus and mucus plugs.”
Dr. Ehle and his team did as many as four bronchoscopies a day. “Some days it seemed like I would just go right from one person to the next doing these procedures,” he said. “We got very efficient.”

“In the pre-COVID days, the process to set up for these procedures could take an hour, explained Ehle.” Over time, we adapted and endoscopy brought in disposable scopes on a portable cart. So all we need is a respiratory therapist, myself and a nurse, which made a very long procedure significantly shorter. From start to finish, it might take 20-30 minutes, depending on the complexity.”
The pandemic forced everyone to think differently. Listen as Michelle Gamble remembers being surprised and impressed by what she saw on one occasion.

Emotionally exhausting

Sometimes the most emotionally draining part of the day was having difficult conversations with families. “Any conversation about a person’s imminent dying is challenging,” said Dr. Jack Lyons, Intensivist. “Those conversations are markedly more difficult on the telephone. And as the pandemic progressed, the amount of misinformation circulating through the public also progressed.”
This led to more requests for non-conventional therapies, such as Ivermectin.

“Sometimes these requests were polite, but other times there was clear mistrust of the established medical community,” said Dr. Lyons. “And sometimes they included veiled threats. That’s where the Hippocratic Oath becomes central – to first, do no harm. Studies showed these therapies don’t help and they carry some risk of toxicity. So I know that therapy cannot help people and it may harm them. That’s a violation of the central tenet of the Hippocratic Oath.”
“COVID divided everybody,” said Tindal. “What I noticed during the most recent surge was that patients and families were just flat out angry at us.”

“We know we need to allow grace and that some people grieve angry and some people grieve in a confrontational way,” said Dr. Lyons. “Admittedly, it becomes challenging when that’s the norm. It’s one thing to deal with that twice a week; it’s another to deal with it twice in an hour. Empathy is something that is actively practiced. It’s a skill like any other and you’re tapping your reservoir, which can only go so deep some days.”

Brighter future
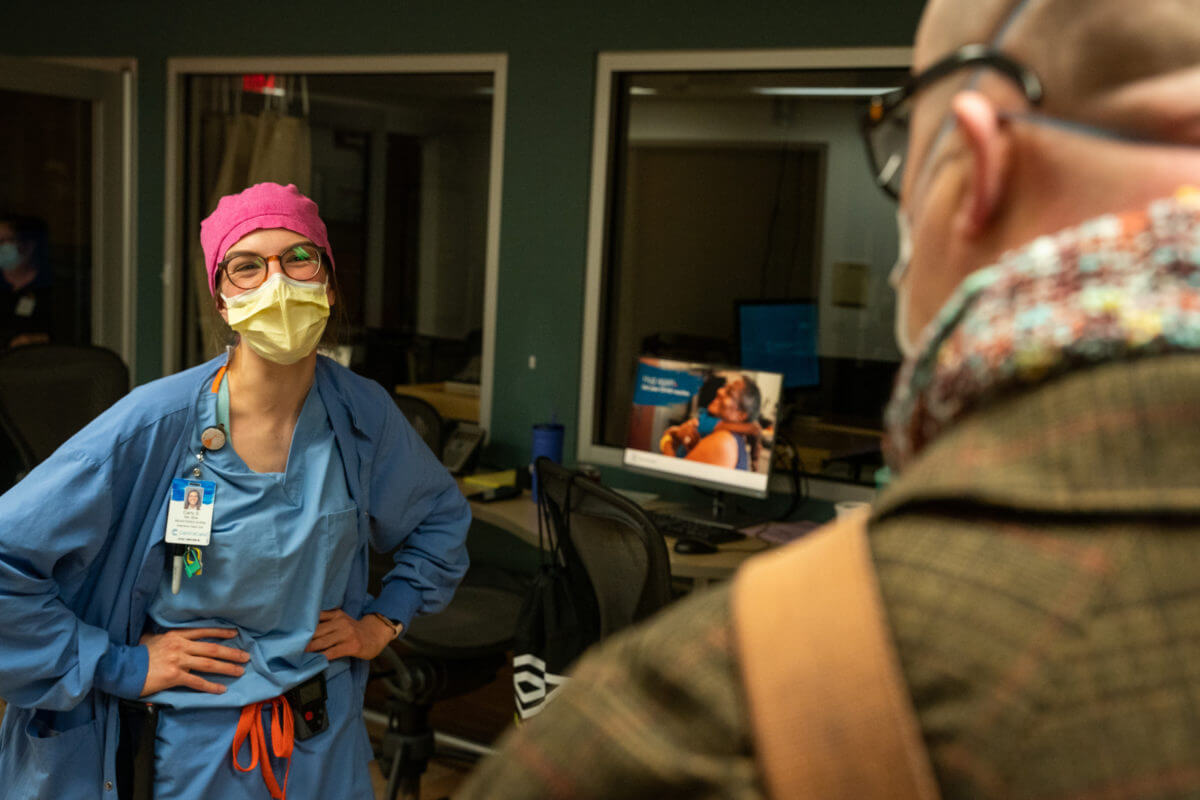
Through it all, the team feels a tremendous sense of gratitude for each other.
“I’m so proud of our team,” said Michelle Gamble. “Most will say they don’t feel like heroes – that they’re just doing their job. But they’re amazing.”
“Our nurses and everyone on the unit worked their tails off and they still are working their tails off,” said Tindal. “Thinking about the future, I want us to be able to walk away from this and have some good things happen. COVID was horrible. People are broken and we need to move forward, but we also need to really sit down, look at what worked, what didn’t work and then begin to move forward.”

Dr. Lyons too is choosing to be optimistic as he looks ahead. “There are a lot of people that are here today because of the efforts of our nursing staff, our respiratory therapists and all our caregivers,” he said. “We knew that we couldn’t help everybody – but for those we could – we did our best and that has to be some part of the healing. We need to acknowledge that things weren’t done perfectly, but we helped a lot of people.”

No Beds: An Impossible Situation




Reading your front line stories, makes me proud to work for CentraCare and helps me understand the employee experience after we recruit and onboard. Thanks for sharing your heartfelt experiences with us!
what a blessing from God all you have been>
Unimaginable. This is the word that comes to my mind as I listen to the stories. I can’t imagine being a patient, a family member nor any of the staff that is doing this work. I can’t imagine what it took & takes to continue to care for patients, families and each other. You have my highest regard. I am grateful to live in a community with such good care and know this is the place I would want to be should I or my family need it some day. Thank you, Thank you all for your dedication.
Incredibly grateful for the dedication and sacrifice made by the team in ICU! <3
This brought back so many memories (and tears) from the past 2 years. I do want to send out a shout to the critical care trained float pool staff. They flexed to where they were needed, often taking some of the toughest assignments. Working alongside the ICU, CICU and ETC staff during the pandemic will be something I will never forget. I look forward to the future where we can all grow and heal.
Thank you !!! (and great photos)
I have said it many times over the years that ICU is the best unit I’ve worked in (I haven’t left since 1983!) because they truly do become another part of your family.
It could be crazy busy, but I’ve never felt alone when working in ICU. Your co-workers ‘have your back’ and many things are done as a team…when a new admit comes thru the door, it seems as if everyone in the unit is there just doing what needs to be done or asking “what can I do to help you?” The same question is asked of their neighboring co-worker throughout the day (or my favorite: “nights”) if someone has an extra moment…everyone helps each other and not just RN > RN, but all members of the ICU “team”.
ICU is a constantly changing environment and everyone is always looking for the best way we can care for our patients and their families…Going ‘above and beyond’ is the norm in the life of the ICU!
Your work is the similar to war heros: no choice but to work with amazing grit in horrible circumstances. You provided care as if the patient was Christ himself. Blessings
There are so many incredible stories of teamwork, dedication, hope and healing throughout these stories and pictures. I am so proud of this team and all of the efforts which they have put forth!
I cannot even start to understand how difficult things were for the staff and providers in the St Cloud ICU during the Covid surges. What amazing team work, sacrifice and hard work. We are blessed to have the team we have