no beds
An impossible Situation
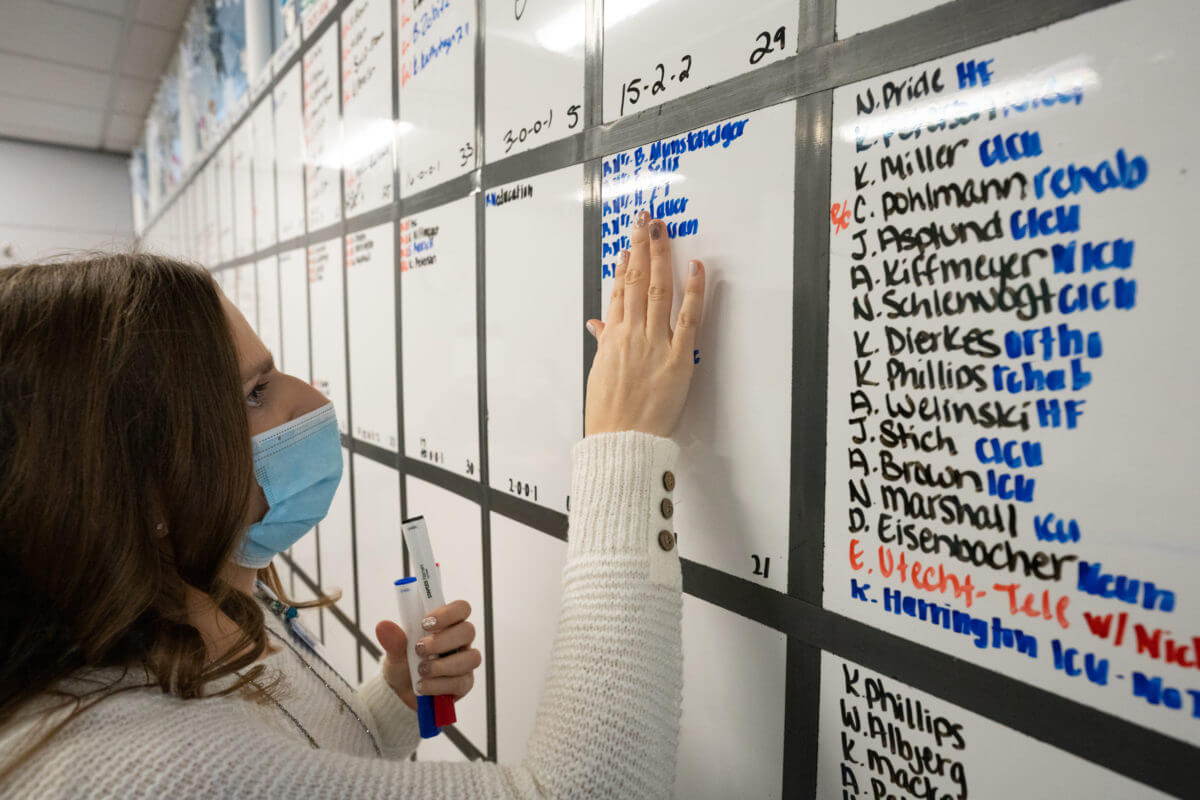
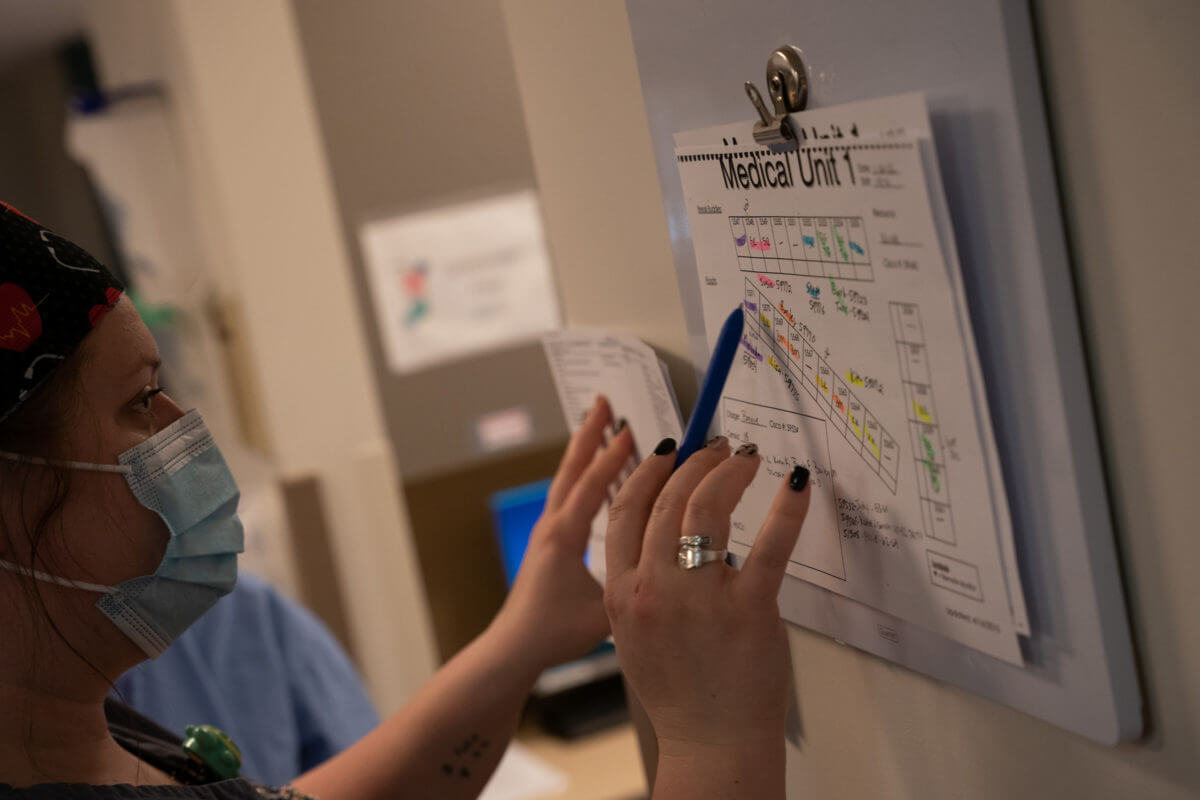
The work was like a complex puzzle – with nursing supervisors attempting to move all the pieces into the right places.

Nursing supervisors have a unique view of the hospital – they communicate across care units and can see where staffing is low and where there’s a surplus. During COVID, St. Cloud Hospital’s nurse supervisors were faced with an impossible situation; how to provide beds and nurses for critically ill patients, when those resources simply didn’t exist?
With St. Cloud Hospital being a hub for specialized care in the region, a big part of the nursing supervisor role is taking in patients whose medical needs exceed what a local hospital can provide.


“I’m trying to figure out, ‘Am I going to get enough discharges today to be able to get these patients in?’” recalled Administrative Nursing Supervisor Karen Neis. “‘We have another COVID patient, but I don’t have another COVID bed – where can I put this patient? I have people from outside facilities with sick intubated COVID patients – they need to come here to a higher level of care, but I don’t have a bed. How do we make this happen? And a lot of times we couldn’t get the patients here. That was heartbreaking for all of us working as supervisors – it was really difficult.”

Strain

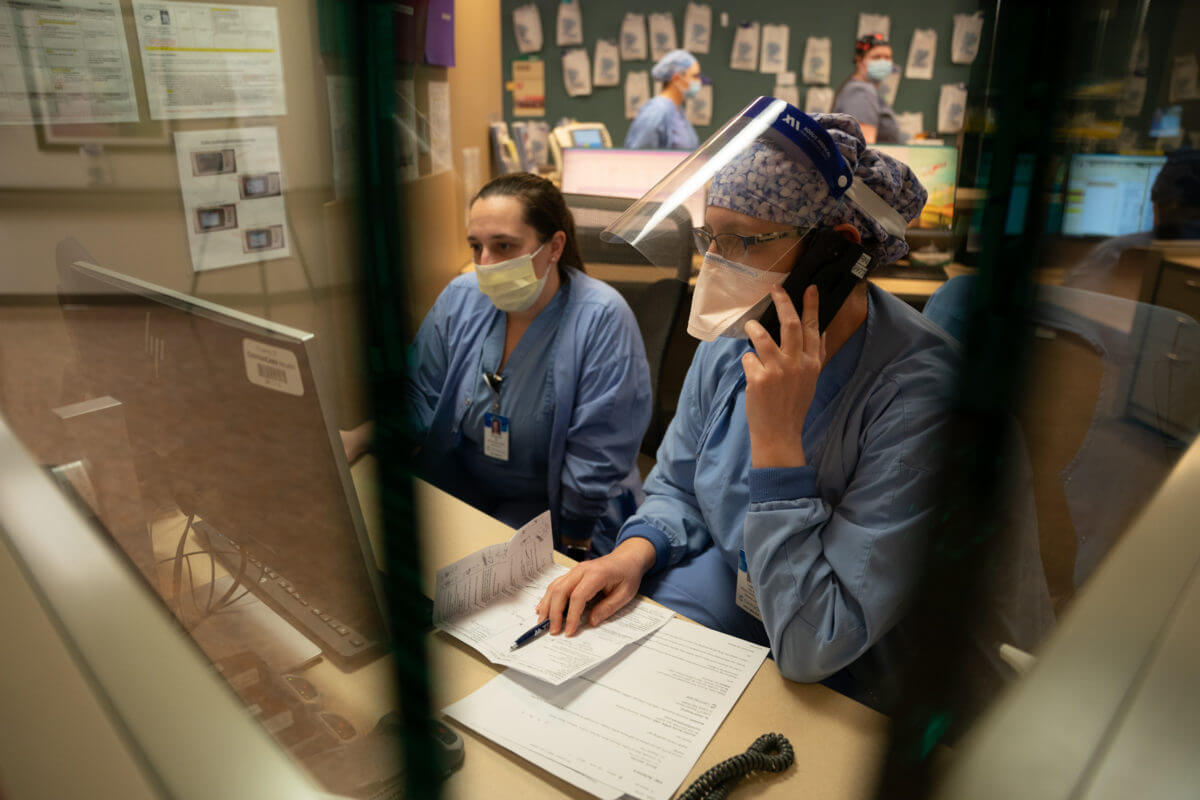
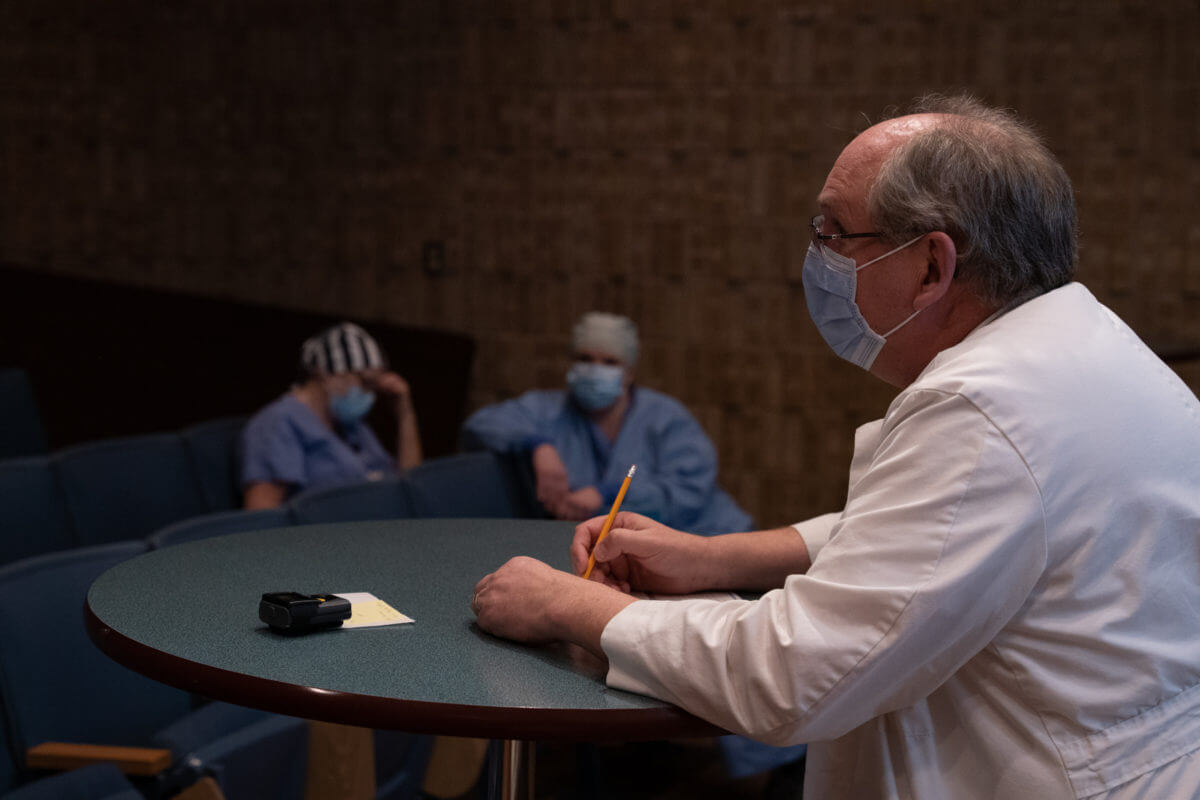
Phones were ringing nonstop as doctors around the region pleaded with nurse supervisors to take on more critical patients. The work was like a complex puzzle – with supervisors attempting to move all the pieces into the right places so that everyone had what they needed. All while the hospital was strained far beyond its capacity.
“The house supervisors are the nurses that run the show at St. Cloud Hospital,” said Tom Schrup, MD, Chief Physician Officer. “They tend to get all of the crises in the region coming their way. There were no beds and regional hospitals and hospitals in other states were calling, begging for us to help them. To not be able to do that was extremely painful. And yet despite that, they held up their professionalism and compassion over and over again.”

COVID also required more of our staff to care for an individual patient.
“It was trying to reshuffle and reallocate staff,” said Zach Brausen. “It was talking to units and saying, ‘Hey, I could really use a nursing assistant, which would free up this RN, which would then help me here – can we make that work? Does that still seem safe?’ Because at the end of the day I want everyone to be safe. And I would always end with ‘I will not do this, if this is not safe.’”
Even if a supervisor was able to solve a staffing problem and get another patient in, the relief was only temporary – particularly when it came to ICU beds.


Uncertainty

“You never were sure that was going to be the last ICU patient that needed a bed,” said Administrative Nursing Supervisor Paul Reisdorf. “So you would give up this ICU bed, and then all of a sudden you have a COVID patient that’s on heated high flow and needs to be intubated. And then all of a sudden, there’s two more that pop up – one from the ER, and one from inside the hospital.”
As staff called in sick, took time off to homeschool children, or resigned their jobs out of fatigue, the hospital became increasingly short staffed across the board. To help, many often stayed far longer than they were scheduled.

“The hardest part,” said Susie Reitmeier, “is asking people to stay and knowing some of these nurses have been here 16 hours. They’re just tired and burnt out and they have to wear their masks and a gown their whole shift. And they’ve seen death – they’ve seen death every day.”


teamwork


After weeks of trying to parse out care, St. Cloud Hospital eventually had to divert all outside bed requests. Overwhelmed with patients coming through the ER, taking on any more was no longer safe.
“It is really hard to say ‘no’ when you know that you have the facility that they need, the higher level of care, the physician, everything!” said Rolee Petersen. “But you just can’t make it work, because of staffing or because of a bed issue.”

There were bright spots amidst the chaos and exhaustion; the nursing supervisors team put up an “Envision 2022” wall where they still post positive images and ideas to help them look forward. And the critical care needs of the regional hospitals inspired the creation of a new role – the Medical Officer of the Day (MOD) – to help triage urgent care.
“I feel like there are a lot of great things that came out of this,” reflected Haley Wipper, RN. “We created processes such as the MOD huddles, which improved teamwork across our system. We had critical care nursing advice calls to help strengthen our critical access to hospitals that didn’t have those resources. We adapted to the labor pool. We just came up with great ideas on ways to get through this using the resources that we had and doing what we could.”

Presented with an impossible situation, the nursing supervisors learned just what they were capable of. And it was far more than they could have ever imagined.










Thank you for the glimpse inside your response. As a regional healthcare coordinator for the West Central region – i want to thank you all for your hard work. My hospitals relied so much on St. Cloud Hosp and i know that it was hard to turn away patients from the smaller sites HOWEVER you never really turned them away – you offered up advice and guided the facilities to care for those patients. My hospitals appreciated all the steps you took to help save lives and they were not just the lives of the patients in house at SCH that you saved. I am so very grateful to each of you!
Some of the best nurses I know are here at Centracare. You guys and gals rock.
What an amazing show of dedication. We are so blessed to have such a remarkable group of people. Thank you for all you have done and continue to do!