regionals
miles apart but at the center of everything
Counted on by their communities, regional hospital teams stepped up in remarkable ways.

As COVID-19 first approached the Midwest, CentraCare put a plan in place; all COVID patients would be sent to St. Cloud Hospital for treatment, leaving regional care centers free to focus on their usual spectrum of services. It made sense at the time.
Cindi Gronau, MD, serves as the Hospital Chief of Staff in Redwood Falls; she remembers how quickly the plan had to be abandoned.


“We had an outbreak at a nursing home, and there was no staff to take care of the residents except for maybe one,” recalled Dr. Gronau. “So the state came in and basically told them that they needed to disperse the patients. We received 15 COVID positive patients [out of a total of 40], and we had no idea what we were going to do with them.”

reaching out
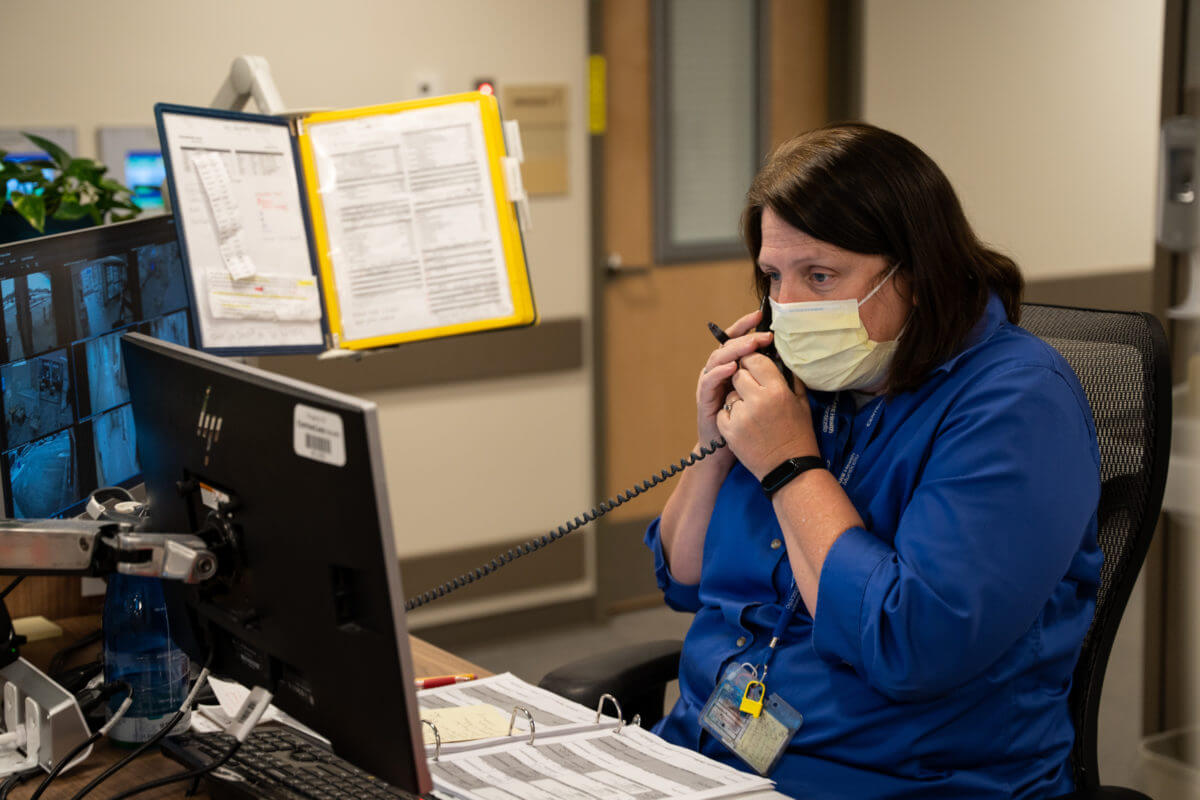

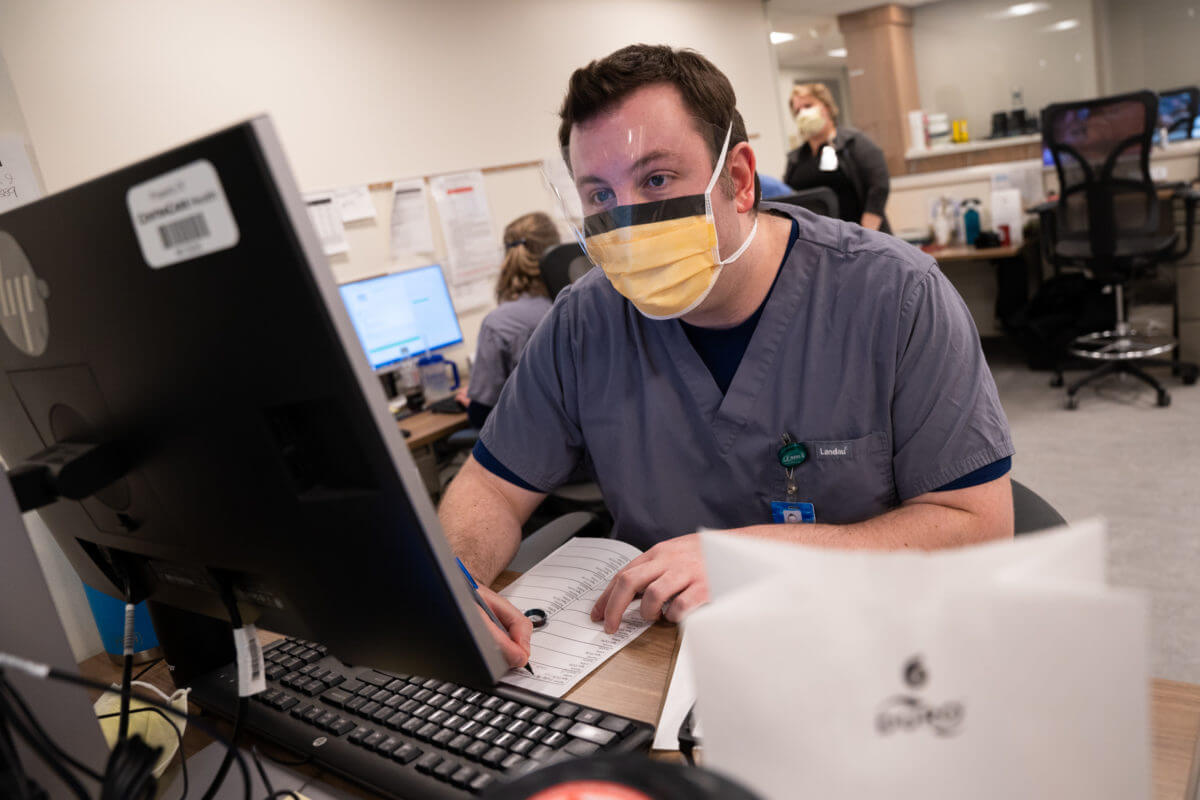
As St. Cloud Hospital quickly filled with COVID patients, doctors and nurses at regional hospitals were spending more and more time on their phones trying to find a free bed for a patient in dire need of treatment, whether it was for COVID or something completely unrelated but equally critical.
“Those days of calling around to every hospital and system in the state and in South Dakota and North Dakota to say, Do you have a bed? We can’t take care of this patient. He needs more than we’re doing. It just was so frustrating and difficult,” said Ulrika Wigert, MD, family medicine physician in Sauk Centre.

With no other options available, nurses and physicians across the region were suddenly put in the position of learning to look after critical patients. Some had never done it before – others hadn’t done it in decades.
“In a small hospital, we have a number of young nurses – that’s often their first job out of training,” explained Deb Peterson, MD, family medicine physician in Litchfield. “They needed to feel like they were doing a good job when it felt to them like they really weren’t, because they felt like they were in over their head. So [I] was cheerleading along with taking care of the patients, when often I was also scared, because they were some very, very sick people.”


personal connection

Adding to the challenge of learning and providing new methods of care was the fact that staff in our rural areas were treating people they knew personally.
“Unique to rural frontline health care workers is that in a small community, everybody knows everybody,” said Cindy Firkins Smith, MD and Senior Vice President of Rural Health. “So the person who’s coming in and is critically ill is oftentimes your neighbor, your kid’s friend’s parents, your family member. And so you’re not only trying to save someone’s life, but you’re trying to save someone’s life that you know, and you love and you care about and you live beside, and it creates an another layer of emotion, commitment, fear, and distress when you feel like you can’t do enough.”


Designated nurses and doctors studied specific procedures, such as intubating, and then trained the other members of their team. For staff who were used to moving critical cases out of the building as quickly as possible, keeping those patients on site was both a mental and emotional challenge.
“Normally in our small facility, if you had anything major – a trauma, heart attack, or severe pneumonia – you call the bigger hospital and they take them. You send them on the helicopter, and away they go,” said Dr. Gronau.


In those instances, staff knew the patient had been given the best care possible. Now that patients had to stay in Redwood Falls, Dr. Gronau said she was sometimes paralyzed by the idea that she might end up doing more harm than good.
Lance Lothert (Respiratory Therapy manager) and Tom Bruns (CRNA) would say, “But if we do nothing, they’re gonna die. We gotta try.”

roles reversed


Regional care centers that were used to turning to St. Cloud for help were now finding their roles reversed. In November and December of 2020, Sauk Centre became an “all COVID” hospital, taking on the patients that needed oxygen, but didn’t require a ventilator, so that St. Cloud Hospital could focus on the more critical cases.
In the early days of the pandemic the surrounding communities were supportive of their healthcare workers. But as political rhetoric inserted itself into public health, patients and their families became less appreciative and increasingly distrusting.

“There was such a huge disconnect with, ‘I’m not going to get vaccinated, I’m not going to wear a mask, but darn it, if I get sick, take care of me,’” said Dr. Peterson. “This was about doing something for the common good and understanding that resources are finite. That’s the part that was hard for me – that people just didn’t understand that.”
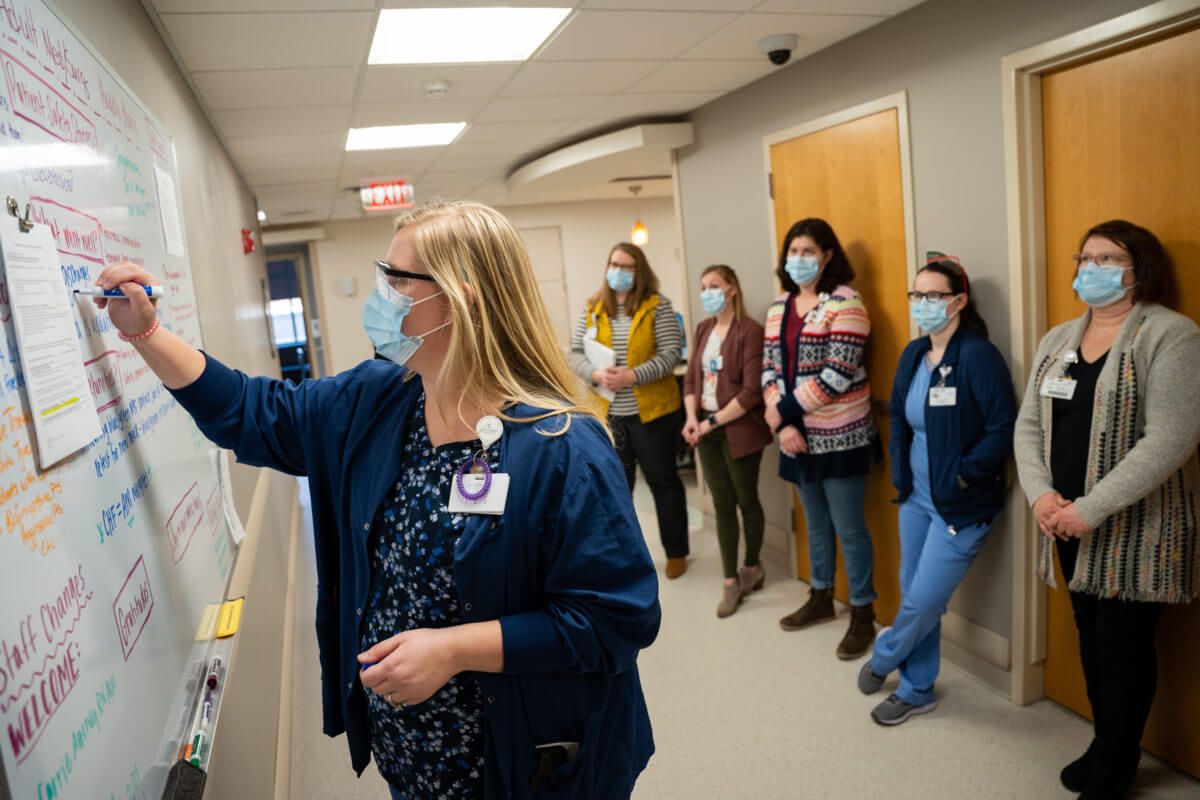
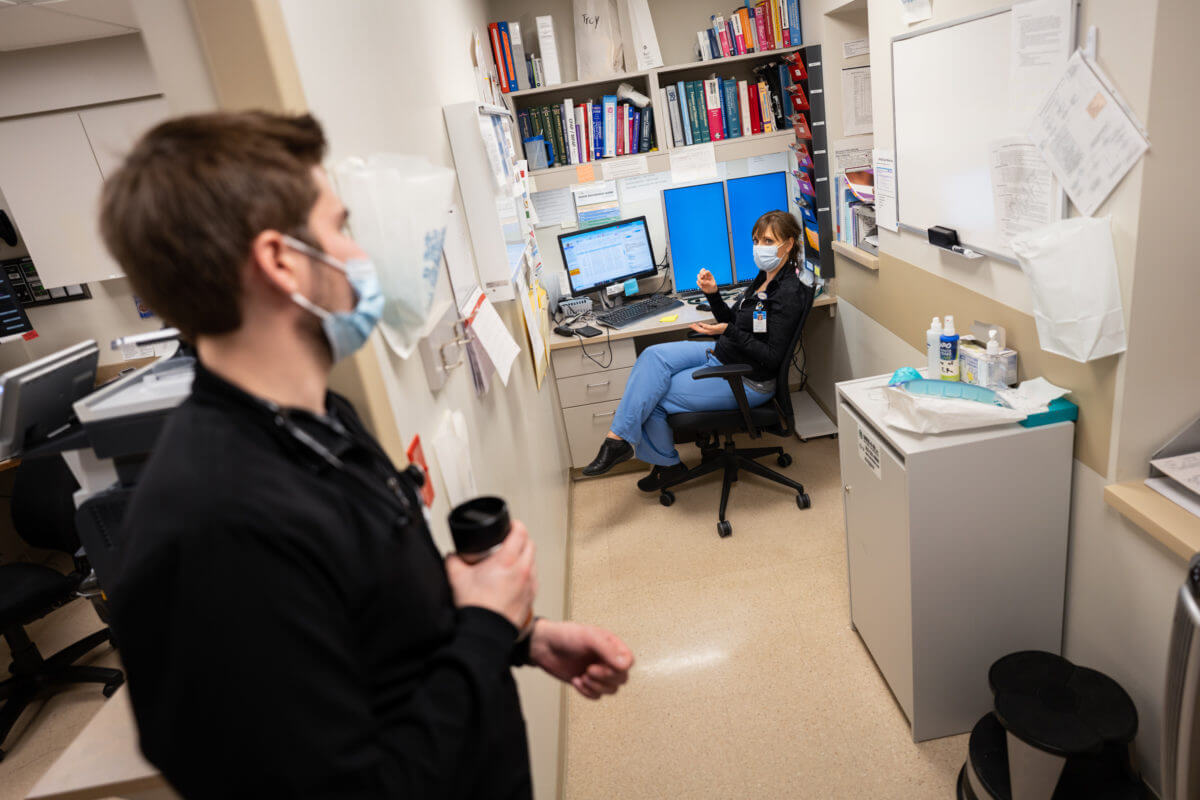
As the pandemic continued, the regional care teams learned a tremendous amount, and became more comfortable caring for critical patients. They collaborated more closely with St. Cloud Hospital, which led to multiple new methods for sharing resources and expertise across the system, through efforts like the Medical Officer of the Day (MOD) and the Rapid Emergency Team.



humbling
Angie Paschke, APRN in Sauk Centre, says the communication and continued teamwork has been awe-inspiring.
“I think that’s been the most humbling part to me. My nurses, good lord, the amount of stuff they’ve learned. The fact that people will call you and check on you. ‘Are you okay today?’ Oh my gosh, the thought that the hospitalist called to check on me today from St. Cloud. It’s huge for me as an APP and certainly I think as the physicians, it just helps create that more collaborative care of our patients. And that’s what I see as the future of CentraCare. It’s teamwork.”
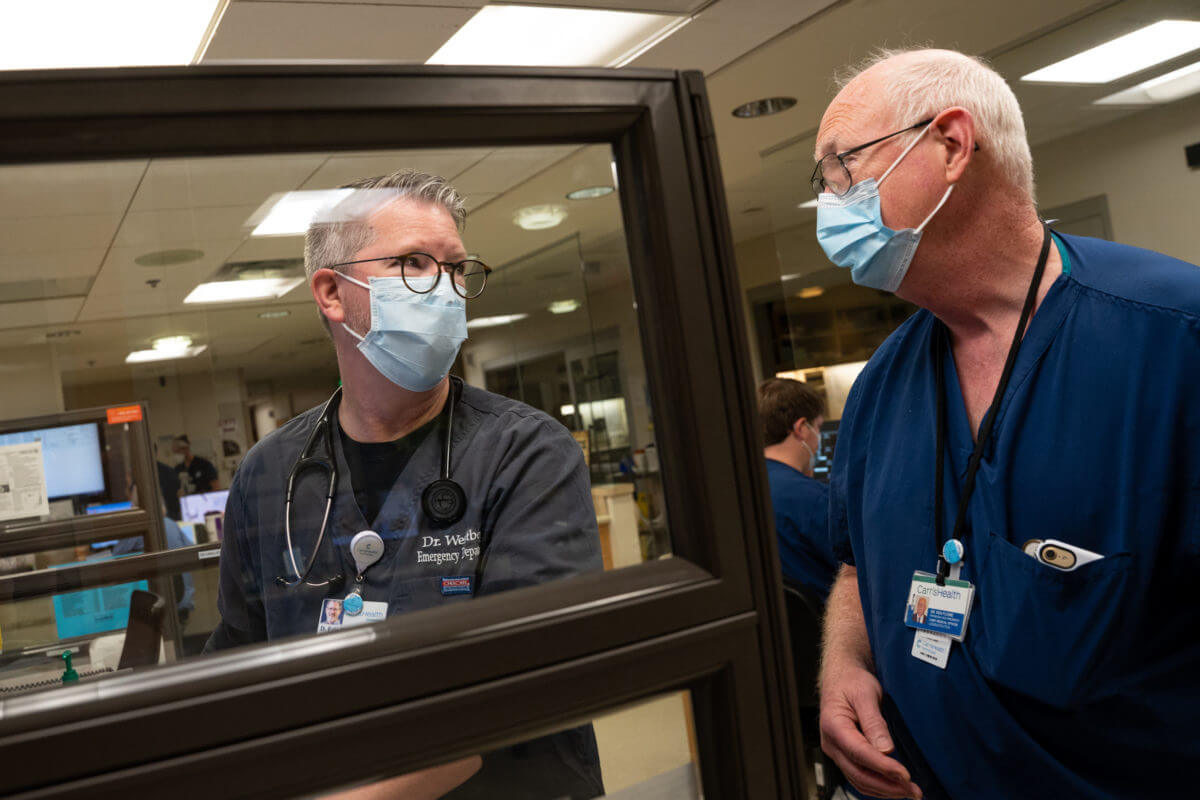
Dr. Peterson agrees.
“I think that what I learned and what my colleagues learned is that we are better together. Having a team is better than standing alone,” said Dr. Peterson. “And that’s a big deal in medicine, because we’re trained to be very autonomous and just do our thing and not ask for help and suffer in silence. And this has been so much better.”










Wow wow wow. Thank you thank you thank you for all your amazing, challenging work.
This is a GREAT article. Thanks for sharing.
Great work!